Burundi achieves the 95-95-95 targets in the fight against HIV/AIDS
- April 6, 2023
- HIV/AIDS / WCA
- By The Bureau
- Read in French

 Burundi is among the few countries in West and Central Africa to have achieved the 95-95-95 targets in the fight against HIV/AIDS/STIs, thus ranking second after the Kingdom of Eswatini. This means that in Burundi, 95% of all people living with HIV are aware of their status, 95% of those aware of their status are on treatment, and 95% of those on treatment have achieved viral load suppression.
Burundi is among the few countries in West and Central Africa to have achieved the 95-95-95 targets in the fight against HIV/AIDS/STIs, thus ranking second after the Kingdom of Eswatini. This means that in Burundi, 95% of all people living with HIV are aware of their status, 95% of those aware of their status are on treatment, and 95% of those on treatment have achieved viral load suppression.
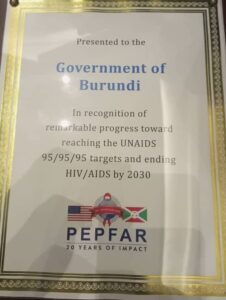
Due to this tremendous progress, the country was commended by PEPFAR for its efforts to combat HIV/AIDS, the results of which were expected to be attained by 2030.
.Find out how they succeeded through four key points
The main cross-cutting factors that contributed to attaining the 95-95-95 targets in Burundi include:
-
Political commitment:
The First Lady, Her Excellency Mrs Angeline Ndayishimiye, has been intensely involved both in the HIV response and resource mobilisation, which has allowed continuous implementation of interventions. This political commitment was also manifest through the invaluable support from technical partners, who worked in close collaboration and synergy to achieve the targets. Worth noting is the responsibility of the Ministry of Health in rapidly adopting and implementing the WHO guidelines, in particular the “test, treat and track everyone” approach, using an implementation plan.
- Decentralisation of care and delegation of tasks: the policy of delegating tasks was effective. It was followed by health system strengthening, particularly the strengthening of the technical platform and the capacity building of healthcare providers at all levels. The policy of decentralisation of care was first applied to adults in 2012, then extended to children in 2018. In 2019, the delegation of tasks for ARV treatment was also extended to children. As a result, the number of Treatment Centers increased from 512 in 2016 to 885 in 2020. This increase allowed for better coverage of the entire country and gave patients easy access to care. By adopting the decentralisation and delegation of tasks approach, Burundi has enabled a wide range of health facilities (both those in the public sector and those in the community) and healthcare providers to meet the needs of people living with HIV. This strategy allows for efficiencies in the health system to provide comprehensive, patient-centred care and to reach the underprivileged.
- Commitment of the civil society: the civil society involved in the fight against HIV has played a leading role in developing and implementing differentiated approaches to prevention, testing, treatment and care. The setting up of the Cadre Consultatif et Décisionnel des Organisations de Personnes vivant avec le VIH (consultative and decision-making framework of organisations of people living with HIV) has ensured greater involvement of people living with HIV and good coordination of the work of organisations of people living with HIV, particularly in advocacy. This commitment, especially on the part of people living with HIV, empowers them to fight against the stigma related to HIV/AIDS and demonstrates their resilience. Besides people living with HIV, innovative practices have facilitated access to services by key populations confronted with socio-cultural, structural and legislative barriers.
- The availability of inputs: testing inputs and ARVs made it possible to carry out all activities without difficulty. This played an important role in ensuring the continuity of services and in motivating the actors.


